Hormone Replacement Therapy in Menopausal Women
Oct 30, 2023
Imagine there was a drug, an approved, inexpensive, and extensively tested medication that could:
- extend your life by more than 3 years,
- decrease the risk of heart attack or stroke by 50%
- decrease the risk of breaking a bone by 35 to 50%, and
- decrease the risk of dementia by 35 percent.
Wouldn’t you want to know about this drug?
What if I then tell you that this drug used to be widely prescribed but that doctors are now reluctant to prescribe it because of unwarranted fears about the risks? And what if I further explained that these fears are due to bad science, science that was influenced by the researchers’ preexisting ideas even in the face of contradicting evidence?
How Medical Research Can Harm Us
I find it sad to be writing about yet another area of medicine in which bad science has caused harm. In a previous blog, I described how we became culturally brainwashed that dietary fat is bad for us. I described how the early studies by Ansel Keys were misinterpreted by the big companies that produce seed oils and how for 70 years our health has suffered from misguided recommendations to eat a low-fat, high-carb diet.
I have written repeatedly throughout my career about how the field of Myalgic Encephalomyelitis / Chronic Fatigue Syndrome (ME/CFS) has been misled by those who promote cognitive behavior therapy (CBT) and graded exercise therapy (GET) as treatments when, in fact, these approaches make most people with ME/CFS worse.
The story I'm going to share with you in this blog has similarities to these two other stories. Researchers had a pre-existing belief that estrogen caused breast cancer, and instead of doing a study to prove themselves wrong (as is the gold standard in science), they dug deep to find data that appeared to support their belief. The negative health impacts of this story are just as severe as those of the low-fat diet craze and the CBT/GET recommendations for ME/CFS.
The drugs we are talking about are estrogen and progesterone, and the therapy is hormone replacement therapy (HRT) for women in their menopausal years.
You may be wondering why I’m writing about HRT and what its relevance to ME/CFS and related diseases is. Many of my patients have had significant hormonal-related symptoms throughout their lifespan which has increased their overall misery and disability. As a general rule, the more symptoms which can be adequately managed, the better our quality of life.
For this reason, I’ve been learning more about how to live healthier for longer. Many of the hallmarks of aging are relevant to ME/CFS, FM, ES, long COVID, and chronic pain. So, learning about healthy aging may be helpful to many of you.
Before I dive into the story, here are a few notes on terminology. Hormone replacement therapy refers to the use of estrogens and progestogens to replace the hormones no longer being produced by the body either due to menopause or ovarian surgery. For women who have had a hysterectomy, estrogen can be used alone. For women who have a uterus, estrogen and progesterone need to be used together to prevent an increased risk of uterine cancer from unopposed estrogen.
Today most women on hormone replacement therapy use bioidentical hormones, meaning the same molecules produced by women’s bodies. These are various formulations of estradiol and micronized progesterone. But, back when the studies discussed in this blog were undertaken most women were using non-bioidentical molecules — conjugated equine estrogen (CEE - brand name Premarin®) and medroxyprogesterone acetate (MPA - brand name Provera®). For simplicity, I will use the terms estrogen and progesterone in this blog.
A Brief History of Hormone Replacement Therapy
When I was in training in the 1980s and early ’90s, hormone replacement therapy (Premarin® and Provera®) was widely prescribed for perimenopausal and postmenopausal women. Like many aspects of women’s health, we weren't taught about it in our training. As a result, I remained pretty ignorant about the potential risks and benefits of hormone replacement therapy (HRT). Being young at the time, I didn’t feel pressed to learn more. Early in my practice, I remember telling patients that I would learn more about this topic as I aged. Well, now I'm turning 60 and am much more interested.
To learn more, I listened to an interview with Dr. Avram Bluming and Carol Tavris, PhD, on The Drive podcast with Dr. Peter Attia. I was so blown away by the research-based statistics they were sharing that I had to learn more. So, I read the book Oestrogen Matters by the same authors, and then numerous papers, and guidelines trying to understand how there can be such diversity of opinion based on the same data.
During my career, I was reluctant to prescribe hormone replacement therapy to asymptomatic perimenopausal and postmenopausal women. I reasoned that menopause is a natural process that doesn't require medical treatment. Bluming and Tavris corrected my thinking on this early in their book. They explained that living to 80, 90, or even 100 is not “natural” for humans. Until the advent of hygiene and antibiotics, it was a rare event. Now that the average life expectancy for a Canadian woman is 81.6 years, most women will be living a significant portion of their lives postmenopausal. The question of whether we will live healthier and longer with or without hormone replacement is important.
HRT has two possible uses:
- to treat the symptoms associated with menopause (more on this below) and
- to delay the onset of chronic health conditions in healthy postmenopausal women. This is called primary prevention.
Much of the information in this blog was inspired by Bluming and Tavris and the over 300 papers referenced in their book, Oestrogen Matters. Where I have gotten information from other, more recent sources they are referenced with hyperlinks.
How Did the Women’s Health Initiative Study Get it so Wrong?
Based on large observational studies in the 1980s and ’90s, it was thought that HRT might lessen the risk of heart disease, stroke, bone fracture, and dementia but possibly increase the risk of breast cancer. Observational studies cannot prove causation so there was a need for a prospective randomized trial to see whether the observational findings could be validated. This was the rationale in the early 1990s, the Women's Health Initiative (WHI) study, the most expensive clinical trial in U.S. history costing close to 1 billion dollars.
The results of the WHI study were first published in 2002 in a flurry of media releases sensationally reporting that hormone replacement therapy increased the risks of breast cancer, heart disease, dementia, and decreased lifespan. No positive effects were reported. The study was stopped 3.3 years prematurely due to these reported harms. I remember the fear generated by the announcement that estrogen increased breast cancer estrogen risk. Bluming and Tavris explained that although this belief (just like the belief that dietary fat causes heart disease) continues to be widely held, it is incorrect.
Does Hormone Replacement Therapy Increase the Risk of Breast Cancer?
 Of 45 studies published between 1975 and 2000, 82% found no increased risk of breast cancer in women using hormone replacement therapy. Prior to the WHI study, the consensus was “on the basis of the available evidence we recommend that all postmenopausal women be considered candidates for hormone replacement therapy and be educated about its risks and benefits.” Within one year of publication of the WHI study, more than half of the 6 million women in the USA who were on HRT abruptly discontinued the treatment. Many weren’t given a choice by their doctors.
Of 45 studies published between 1975 and 2000, 82% found no increased risk of breast cancer in women using hormone replacement therapy. Prior to the WHI study, the consensus was “on the basis of the available evidence we recommend that all postmenopausal women be considered candidates for hormone replacement therapy and be educated about its risks and benefits.” Within one year of publication of the WHI study, more than half of the 6 million women in the USA who were on HRT abruptly discontinued the treatment. Many weren’t given a choice by their doctors.
However, the connection between hormone replacement therapy and breast cancer is contested. Unlike the clear connection between smoking and lung cancer, the connection between hormone replacement therapy and breast cancer doesn't fulfill any of the widely regarded Bradford Hill criteria of causality. Here are just a few interesting facts:
- Breast cancer increases in incidence after menopause when estrogen levels are decreasing, not during pregnancy when estrogen levels are sky high.
- High-dose estrogen has been used effectively to treat metastatic breast cancer.
- Some normal breast cells have estrogen receptors on their cell membranes. Women fear that this means estrogen causes or makes their cancer worse. But, in reality, estrogen receptor positive (ER+) cancers are slower growing and have a better outcome than ER-cancers.
- Women who are on HRT at the time of a breast cancer diagnosis live longer than those who are postmenopausal and not on hormone replacement therapy.
The increase in breast cancer incidence in the WHI study was only about 1/1000 women and was not clinically significant. And deaths due to breast cancer did not increase at all. Meanwhile, fewer women on HRT die of breast cancer than from the big killers: heart disease, osteoporosis, and dementia, and in certain circumstances, hormone replacement therapy can positively influence these three big killers. More on this later in this blog.
Does Hormone Replacement Therapy Reduce Menopause Symptoms?
So, let’s start with the use of HRT, to treat the symptoms of menopause. When women stop having menstrual periods, the ovaries stop producing estrogen and the levels of estrogen and progesterone plummet within a year to less than 1% of the young adult levels. Eighty percent of women experience some symptoms with menopause, and the average duration of symptoms is 7.4 years or longer. Many women seek help for these symptoms from their physicians. The most common symptoms of menopause are:
- hot flashes
- night sweats
- insomnia
- cognitive problems
- vaginal dryness / painful intercourse
- bladder problems like frequent and painful urination
- depression and anxiety
- aching joints
- palpitations
- weight gain
Virtually all authors agree that hormone replacement therapy is the most effective treatment for menopause-related symptoms and that it can significantly reduce suffering and increase quality of life. Due to the WHI reports, however, many women fear hormone replacement therapy and want to try alternatives to hormones. The North American Menopause Society published a comprehensive review of alternatives to hormones and concluded, “Hormone therapy remains the most effective treatment for vasomotor symptoms and should be considered in menopausal women within 10 years of their final menstrual periods.”
Does Hormone Replacement Therapy Increase Life Expectancy?
And there’s more. Studies have suggested that HRT can not only significantly decrease the symptoms related to menopause but can decrease risk of serious chronic conditions that kill women, such as cardiovascular disease, bone fracture related to osteoporosis, dementia, and something called all-cause mortality. The use of hormone replacement therapy to prevent the big killers is called primary prevention — preventing illness before it starts. For women who don’t have serious symptoms of menopause, using HRT for primary prevention is more controversial because otherwise healthy women have less tolerance for side effects.
Is Hormone Replacement Therapy Good for the Heart?
To put things in perspective, the number of women who die each year of heart disease is more than seven times the number who die of breast cancer. In every decade of life, more women die of heart disease than breast cancer. Even women who have had breast cancer are more likely to die of heart disease. It is well known that women's risk of heart disease increases with menopause. This is widely believed to be because estrogen has a protective effect on the heart and blood vessels. But that doesn't necessarily mean that supplementing with estrogen and/or progesterone at menopause will lessen the risk. A Danish study published about the same time as the WHI study reported a 50% decrease in acute cardiac events, like heart attack, in women taking either estrogen or estrogen plus progesterone.
 A comparison of the results from the decades-long observational Nurses’ Health Study and the WHI study may help us understand what is going on. In the Nurses’ Health Study, the use of estrogen replacement correlated with a lower rate of heart attack, whereas in the WHI study, risk of cardiovascular events increased. The increased risk was only about one additional case per thousand women treated and was not statistically significant.
A comparison of the results from the decades-long observational Nurses’ Health Study and the WHI study may help us understand what is going on. In the Nurses’ Health Study, the use of estrogen replacement correlated with a lower rate of heart attack, whereas in the WHI study, risk of cardiovascular events increased. The increased risk was only about one additional case per thousand women treated and was not statistically significant.
This comparison paper showed that the age at which hormone therapy is started seems to make a difference. The risk of cardiac events is decreased in women who start hormone replacement therapy between the ages of 50 to 59 but is slightly increased in older women. And women using estrogen plus progesterone have more cardiac events than women on estrogen alone. Over time, the WHI authors changed their findings and, in 2007, reported that women who started HRT within 10 years of the onset of menopause had a decreased risk of heart disease. But these later reports didn’t get the fanfare of the original press release.
Unfortunately, the manner in which the WHI results were reported had significant negative outcomes for women. A group of Finnish researchers studied the effects of discontinuing hormone replacement therapy after the WHI publication in 2002. They found that the death rate from cardiac causes doubled in those who discontinued hormone therapy compared to those who stayed on HRT.
Current thinking is that hormone replacement therapy decreases risk of heart disease for women within 10 years of their last menstrual period unless they have pre-existing heart disease or risk factors. It is thought, but not yet proven, that the transdermal estrogen patches used today are less harmful than estrogen taken by mouth. For women with an intact uterus, bioidentical micronized progesterone (Prometrium®) is recommended rather than medroxyprogesterone acetate (Provera®). The latter progestin was used in the WHI study and is thought to contribute to their findings of increased cardiac risk.
How Effective is Hormone Replacement Therapy for Osteoporosis?
Next, I delved into osteoporosis, a condition for which virtually all studies agree that HRT is beneficial. Bone density and strength reach a peak in women in the mid-30s and then start declining. The rate of decline speeds up with menopause. As bones lose strength, they are more prone to break if a person falls. A broken hip bodes poorly for longevity. For people over the age of 70 who suffer a hip fracture, 20 to 25% die within a year. Women lose on average 3.75 years of life after a hip fracture.
 Most women are familiar with the bone mineral density test and know that, as their Z score on that test decreases (becomes a larger negative number), they’re more at risk for breaking a bone. To protect against osteoporosis, many women take calcium and Vitamin D. I was shocked to learn that neither calcium, Vitamin D, nor the combination decreases the incidence of fractures in post-menopausal women.
Most women are familiar with the bone mineral density test and know that, as their Z score on that test decreases (becomes a larger negative number), they’re more at risk for breaking a bone. To protect against osteoporosis, many women take calcium and Vitamin D. I was shocked to learn that neither calcium, Vitamin D, nor the combination decreases the incidence of fractures in post-menopausal women.
This surprising finding is because calcium increases bone density but not resilience. For bones to be resilient, they need strong, flexible collagen fibers which give them the ability to bend without breaking. Estrogen and progesterone increase bone strength and resilience and are more effective at preventing fractures of the spine and the hip than any other treatment. Even the WHI reported a 33% decrease in hip fractures in women taking either estrogen alone or combined hormone therapy. The bad news is that this protection decreases as soon as women discontinue hormone replacement therapy leading some to claim HRT is not worth using.
Are there alternatives? Weight training is often recommended to prevent or mitigate osteoporosis. Although weight training improves bone strength and resistance to fracture in premenopausal women, it is only effective in post-menopausal women who are also on hormone replacement therapy.
What about the most commonly prescribed medications for osteoporosis, bisphosphonates like Fosamax® and Actonel®? These drugs are part of every osteoporosis guideline as a first line therapy. In the first 5 years of use, bisphosphonates decrease fractures. But after 5 years, they’re associated with a 45X increase in atypical hip fracture. This is because bisphosphonates increase bone mineralization but not resilience. Overall, bisphosphates decrease fractures more than they cause them, but hormone replacement therapy is still the most effective treatment for osteopenia and osteoporosis and doesn’t increase any types of fractures. Sadly, the 2023 Canadian Clinical Guidelines for Management of Osteoporosis mentioned hormone replacement therapy only in passing and emphasized the risks more than the benefits.
A 2023 review of the effectiveness of hormone replacement therapy on bone density and fracture rate concluded that the benefits outweigh the risks in women under the age of 60 or within 10 years of menopause. Like Bluming and Travis, these authors re-evaluated the WHI data and showed that the study found hormone treatment associated with a decrease of between 24 to 34% in fracture rates.
They summarize the impact of hormone replacement therapy on several diseases (see below). The top chart shows the impact of taking conjugated equine estrogen plus medroxyprogesterone acetate on a number of serious chronic health conditions. The bottom chart is the data for women who took estrogen alone. The red boxes above the X axis (horizontal line) represent conditions which increased in the women taking the hormones. The blue boxes below the line show conditions which decreased in the women on hormone therapy. You can see in the analysis of the WHI data (below) that most of the conditions studied show improvements (blue boxes) in the HRT groups.
The authors suggest a strategy to use hormone replacement therapy in the years right after menopause to decrease risk of osteoporosis and fracture. They explain that this will buy time so that, as women age, they can use bisphosphonates later on if they stop hormones and their bone density decreases. They recommend using transdermal estrogen patches if possible and at the lowest possible dose to minimize the risk of blood clots and stroke.
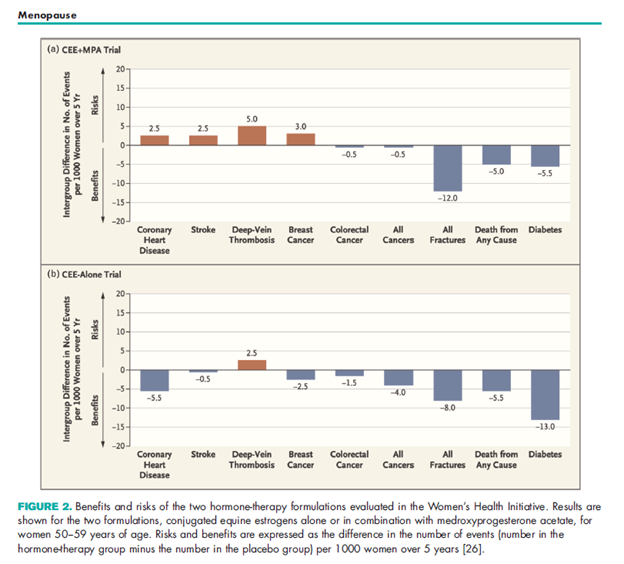
Source: Shah & Ariel, https://dx.doi.org/10.1097/GCO.0000000000000858
Does Hormone Replacement Therapy Affect Brain Health?
Alzheimer’s disease is twice as common in women than men. For some time, it has been thought that this increased risk after menopause may be due to decreased female sex hormone levels. The evidence has suggested that estrogen, in particular, is beneficial for brain health. In lab experiments, estrogen increases nerve growth and plasticity. It increases brain blood flow and decreases the buildup of B amyloid and Tau, two proteins implicated in the development of Alzheimer’s disease.
 Observational studies have shown that women using estrogen replacement have a 40% lower risk of Alzheimer’s disease and 34% lower risk of all forms of dementia. Yet, the WHI study reported a doubling of the dementia risk in women over the age of 65 taking estrogen and progesterone. How can we reconcile these conflicting data?
Observational studies have shown that women using estrogen replacement have a 40% lower risk of Alzheimer’s disease and 34% lower risk of all forms of dementia. Yet, the WHI study reported a doubling of the dementia risk in women over the age of 65 taking estrogen and progesterone. How can we reconcile these conflicting data?
A 2023 analysis suggested that the answer may be more nuanced than a simple yes or no. The WHI study enrolled many unhealthy, overweight women in their 60s and 70s. Many of these women may have already been developing cognitive issues, and estrogen cannot reverse problems that are already in the early stages. Studies show that women who start HRT soon after menopause have a decreased dementia risk, but that risk increases with age and time after the onset of menopause.
These authors suggested that using HRT to improve cognitive health may be warranted if started before age 65 in healthy, cognitively intact women. The addition of medroxyprogesterone acetate (Provera®) in women with an intact uterus diminishes this benefit. It’s not known whether bioidentical progesterone (Prometrium®) will have a similar negative effect.
The U.S. Preventive Services Task Force Reports
Although many organizations worldwide recommend hormone replacement therapy to prevent cardiovascular disease, osteoporosis, and dementia, an influential guideline by the U.S. Preventive Services Task Force has recommended using HRT only to treat severe symptoms of menopause and advised against using HRT for primary prevention.
Given all the data I have mentioned in this blog, how can we understand this recommendation? One possibility is that the task force only considered data from randomized controlled trials and ignored even large, well-designed observational studies. After the WHI study stopped prematurely, most other trials underway followed suit, and no large, randomized studies have been funded since. So, the WHI data continues to have a huge influence on all meta-analyses and guidelines even though it is flawed. It is similar to the outsized influence the PACE trial of CBT/GET has had in analyses of treatment for ME/CFS. Until other large randomized prospective studies are conducted, analyses restricted to randomized controlled trials may not produce valid recommendations.
Conclusions
Based on what I have read, my conclusions are:
- Women should be offered hormone replacement therapy for symptoms of menopause if the symptoms impact quality of life but not if the women are at increased risk for the side effects of HRT, such as blood clots and stroke.
- The treatment is safest and most effective within 10 years (6 years to be very conservative) of the last menstrual period.
- Unlike the U.S. Preventive Services Taskforce, I believe there is a role for using HRT to decrease risk of heart disease, osteoporosis, and dementia.
- If used for primary prevention, hormone replacement therapy is safest and most effective in women who have not yet developed symptoms and who are not at increased risk of the side effects of HRT.
- Although evidence is sparse, bioidentical estrogen and progesterone may be safer than non-human molecules such as equine estrogen (Premarin®) or altered molecules such as medroxyprogesterone acetate (Provera®).
- To ensure quality and consistency, I recommend estradiol and progesterone produced by pharma companies rather than compounded creams.
- Estrogen patches have fewer side effects than when taken by mouth.
- Progesterone is sedating and is best taken at bedtime.
- The effective doses of hormones are very individual.
- It is best to find a prescriber who is willing to work collaboratively to experiment to find the best route and dose to manage symptoms effectively.
If you live in the United States, you can find a qualified practitioner on the website of the North American Menopause Society. Don’t assume your physician will be knowledgeable. Most MDs learn very little about menopause management in medical school.

